Since 2012 government expenses on healthcare have increased substantially. However, the population’s out-of-pocket payments are still significantly high which indicates the government’s inefficient management of funds.
One of the main indicators to measure the efficiency of healthcare expenses is the dynamic of the population’s expenses. As of 2019, the population’s out-of-pocket payments account for nearly 47% of all healthcare expenses which significantly exceeds the average figure of the WHO’s European region’s countries. In 2013-2019, the share of out-of-pocket statement was decreasing annually as a result of growing government expenses on healthcare, although the population’s expenses on healthcare have not really decreased in nominal figures (see Graph 1).
The population’s massive expenses on healthcare are largely related to the purchase of medication. According to the information provided by the Ministry of Healthcare, the share of expenses on medication was 47% out of all out-of-pocket payments. The affordability of medication on the part of the population remains one of the principal challenges of the healthcare sector and it is attributable to higher prices on medication and the minimal coverage of medication funding offered by the state healthcare programme.
Graph 1: Share of Out-of-Pocket Payments of Total Healthcare Expenses

Source: Ministry of Healthcare, National Health Reports, author’s calculations
In the pre-pandemic period from 2013 to 2019, government expenses on healthcare trebled in nominal figures. In this period, the government healthcare expenses to the GDP ratio increased from 1.7% to 2.7%, respectively (See Graph 2). Despite this growth, the government healthcare expenses to the GDP ratio is still low. In 2019, the healthcare expenses to the GDP ratio amounted to 2.7% which is significantly lower as compared to average figure (4.9%) for the Europe region.
Graph 2: Government Healthcare Expenses in 2012-2019
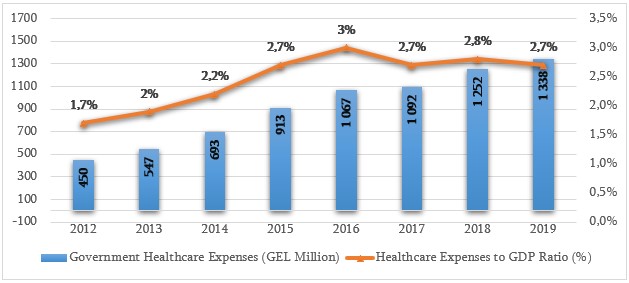
Source: Ministry of Healthcare, National Health Reports, author’s calculations
In 2013-2019, the healthcare budget increased considerably whilst universal healthcare expenses constituted its major portion. In 2013 with the introduction of the universal state healthcare programme, fundamental changes were made in the healthcare system. In particular, the government replaced the targeted principle with a universal one and the state healthcare programme started to cover all citizens who were not using any other health insurance package (of note is that differentiated packages were introduced into the universal healthcare programme later in 2017 and the universal approach was again replaced with a targeted one). The funding rule was also amended – the funding system based on private insurance companies was abolished. The universal state healthcare programme is funded through direct payments from the state budget. The change in the funding rule for the state healthcare programme was assessed negatively at the very beginning. The adoption of a single payer principle puts insurance-related financial risks on the state budget. This practice cannot be considered as an efficient mechanism of expense management.
Statistical data of the previous years show that the government is unable to manage universal healthcare programme expenses. The planned budget of the programme increases annually, although it faces a deficit each year.
In recent years, the government has been focused on capping universal healthcare programme expenses instead of a reduction of the population’s out-of-pocket payments and increasing the affordability of services and medication. It is important that the government change the model and the rule of funding for the state healthcare programme instead of temporary mechanisms to restrict expenses (such as Decree N520). In 2019, the ruling party sought to cap the universal healthcare expenses by Decree N520 of the Government of Georgia issued on 21 November. This decree equalised tariffs for all clinics vis-à-vis high-tech and expensive medical services such as cardiology, cardio surgery, arrhythmology and resuscitation services within the scope of the universal healthcare programme. Decree N520 was a mechanism of a temporary restriction of universal healthcare programme expenses. In addition, it gave rise to a new challenge in the healthcare system. Reduction/equalisation of tariffs on expensive medical services endangers the development of the field – high-tech cardiology. In addition, it induced a new risk that clinics would increase prices on services which are not covered by the universal healthcare system.
On top of increased affordability vis-à-vis medication, the road to the efficient management of healthcare expenses and a reduction of the population’s out-of-pocket payments also requires a bolstering of the primary healthcare element. This would significantly reduce expenses associated with costly hospital treatment and high-tech intervention. The government constantly speaks about primary healthcare reform, although there have not been significant changes and achievements in this regard.